Psychological Interventions to Improve Work Outcomes for People with Psychiatric Disabilities
Morris D. Bell, Jimmy Choi & Paul Lysaker
- Morris D. Bell
- Jimmy Choi
- Paul Lysaker
Many people with severe and persistent mental illness want to be productive and view return to work as a major component of their recovery. This paper presents four psychological interventions that have been used to augment work programs in order to address key issues relevant to finding and keeping employment. The first addresses the problem that clients are often poor at judging their own performance and social interactions on the job. In a weekly group, clients receive accurate feedback about their work performance and set goals for improvement. The second addresses through cognitive behavior therapy the clients’ negative beliefs about themselves as workers and their expectations of failure. The third method uses psychoeducation and social skills training to teach adaptive responses to many common work problems. The fourth approach targets underlying cognitive impairments that make it difficult for clients to learn from their experiences on the job. Using cognitive retraining techniques, clients perform computer-based exercises of attention, memory and problem-solving while they search for and begin working.
Keywords: severe mental illness, schizophrenia, work programs, vocational support
This paper presents psychological interventions aimed at helping people with severe and persistent mental illness to find and keep employment. Four methods are described: accurate feedback, cognitive therapy, social skills training and cognitive remediation.
Funded by grants from the Rehabilitation Research and Development Service, Department of Veterans Affairs to Dr. Bell and to Dr. Lysaker.
Introduction
Inactivity and loss of productive function commonly accompany severe psychiatric disorders (e.g. schizophrenia, other psychotic disorders, mood disorders, PTSD). Yet, surveys (Becker, 2002) indicate that more than 75 % of people with these disorders wish to return to productive activity of some kind. When they attempt to return to work, however, they often have no access to appropriate work activity. They become discouraged when they fail to find a job or fail to keep a job once they get one. As research has shown (Becker, 2002), unemployment itself can lead to deterioration in mental and physical health among previously healthy individuals, and these consequences are all the more serious for those with severe mental disorders.
Vocational services such as supported employment have helped people with severe and persistent mental illness to obtain community-based competitive jobs by finding appropriate opportunities, often with accommodations and supportive services. Supported employment is now regarded as an evidence-based practice (Bond et al., 2002). As pointed out in the Patient Outcomes Research Team national study (Lehman & Steinwachs, 1998), individuals with severe mental disorders have up to now been unlikely to receive vocational rehabilitation services in mental health settings, and the authors strongly recommend that such services should be provided. A manualized version of supported employment for people with severe and persistent mental illness called Individual Placement and Support (IPS) has advanced the implementation of supported employment. A toolkit is available comprised of training procedures for clinical staff, administrators and consumers, a fidelity scale, and consultants to assist in implementation (D. Becker, 2002).
While supported employment appears superior to other types of vocational services for SMI (Clark et al., 1998; Drake et al., 1999; Drake et al., 1996), employment outcomes remain modest. Only about half of those who receive supported employment services achieve competitive employment, and those who do have difficulty maintaining it (Cook et al., 2005). Only about one third are working at any one time, and the job complexity is generally low. Moreover, rates of employment are significantly worse for those with schizophrenia diagnosis (Razzano et al., 2005), which suggests that this large subsample of people with severe mental illness may need interventions that target illness-specific features related to their work impairments.
Therefore, supported employment only partially addresses the problem. It may provide appropriate supports and work opportunity, but patients’ work disability remains apparent. People with severe mental illness in supported employment continue to have difficulty performing their job tasks, and often their interpersonal problems disrupt their work, which leads as many as 50 % to have unsatisfactory job terminations, defined as being fired, or quitting without having other job plans (D. R. Becker et al., 1998; Mueser et al., 2001). In this report, we present psychological interventions to enhance work services, each of which addresses illness- related deficits that cannot be sufficiently overcome through on-the-job supports.
Work Behavior Feedback Groups with Goal Setting
Participants receiving work services meet in a weekly group (usually four to eight workers with a facilitator) for approximately one hour to review on-site evaluations of members’ work performance and to problem-solve and set performance goals for the following week. We (M. Bell, G. Bryson, P. Lysaker, W. Zito, T. Greig, J. Fiszdon, J. Choi) have developed these groups in a number of different settings that include transitional and supported employment programs.
To provide systematic feedback, we created the Work Behavior Inventory (WBI) as a standardized work performance assessment instrument. Detailed information regarding its development, administration and psychometric properties is available elsewhere (Bryson et al., 1997). The WBI is rated by a trained vocational counselor who observes workers on the job and interviews their supervisors. The WBI scales include Work Habits, Work Quality, Social Skills, Cooperativeness and Personal Presentation. These scales were derived through factor analysis, and represent dimensions similar to those from other instruments (e.g. The Work Personality Profile; Bolton & Roessler, 1986). The WBI demonstrated good inter-rater reliability, concurrent validity, factorial validity and discriminant validity. Evidence for predictive validity was also found (Bryson et al., 1999). WBI scores from the third week of work predicted the number of hours worked over a six-month paid work program, with Social Skills, Personal Presentation and Cooperativeness as the best predictors. A composite of WBI scores from their last six weeks of work predicted the number of hours worked and money earned during a six-month follow-up period. These findings indicated that work performance measured by the WBI has a significant relationship to subsequent work outcomes.
In the workers meetings, half the members receive feedback each week, but all participate in problem-solving and goal-setting. The facilitator (usually a vocational specialist or clinician) encourages a process of accurate empathy in which true achievement is acknowledged and praised and problems are realistically confronted. A good deal of social learning occurs as members help each other and learn from each other’s experiences. Each week, members report on their progress toward their individual goals and set new goals, often based on the WBI feedback they have received. Goals might include on-the-job behaviors such as increasing hours of work, being more punctual, being tidier in appearance, taking fewer breaks, or approaching a co-worker about having lunch together. In programs that begin with transitional employment with an expectation of moving on to competitive employment, goals might also include preparing a resume, networking for another job or going on a job interview. There are currently experimental studies underway to determine whether rewards for goal attainment increase vocational outcomes, but results are not yet available.
Rationale
There are several important reasons for believing that regular work performance feedback and goal-setting are especially important for psychiatrically impaired patients. First, severe psychiatric disorders often impair people’s ability to perceive themselves and others accurately. Related cognitive impairments in emotion recognition, theory of mind, attention, memory and executive function can make it even more difficult for workers with a psychiatric disorder to understand accurately what is going on between themselves and their social environment at work. Feedback provides information to workers about their work habits and work quality, but importantly evaluates their social skills, personal presentation, and cooperativeness on the job. These interpersonal behaviors are crucial for vocational success, yet they are not usually addressed directly by supervisors or co-workers in helpful ways. Work supervisors are expected to confront workers who show up late for work repeatedly or who make a lot of mistakes on the job, and they may have good ideas about how to help workers improve in those areas. However, they usually feel reluctant to talk with workers about social withdrawal, odd appearance, or difficulty taking criticism. Supervisors may be uncomfortable with such matters, or out of misguided kindness they may believe that they are doing the person a favor by not saying anything. They may also have no clear idea about how such problems can be remediated. Yet, left alone, these problems can build up until there is a critical incident leading to job loss. Regular and systematic feedback can provide many people with psychiatric disorders a social prosthesis for their impairments in reading cues from their social environment about their interpersonal behaviors, while goal setting and problem solving can often successfully address these issues.
Second, motivation, sense of purpose, and self-confidence can be profoundly affected by psychiatric disorders. Regular feedback provides workers with a psychiatric disorder continual reassurance about what they are doing right as well as what they need to improve on. Since feelings of worthlessness often lead these workers to believe that others are seeing them as inadequate, getting accurate feedback about how they are viewed by their supervisors can reduce mistrust and provide greater confidence in dealing with people at work. By displaying charts showing progress over time, workers are encouraged with concrete evidence of their successes. As goals are set and attained, workers develop greater feelings of self-efficacy and become more willing to attempt new challenges.
Finally, research literature from industrial and organizational psychology strongly supports the effectiveness of work feedback and goal setting for improving individual and organizational productivity. In “Building a Practically Useful Theory of Goal Setting and Task Motivation: a 35-Year Odyssey” (Locke & Latham, 2002), Locke and Latham review the literature on motivation and their experiments in work feedback and goal setting. They conclude with a discussion of the generalization of their theory:
“With goal-setting theory, specific difficult goals have been shown to increase performance on well over 100 different tasks involving more than 40,000 participants in at least eight countries, working in laboratory, simulation and field settings. The dependent variables have included quantity, quality, time spent, costs, job behavior measures, and more. The time spans have ranged from 1 minute to 25 years…In short, goal-setting theory is among the most valid and practical theories of employee motivation in organizational psychology.”
Research Support
Studies published in industrial and organizational psychology and management journals strongly endorse work performance evaluations and feedback to improve productivity (review by Prue & Fairbank, 2002). They also show that combining feedback with goal setting leads to better performance outcomes than when they are not combined (review by Balcazar et al., 1986). Other studies demonstrate that frequent and specific feedback, encouragement of self-appraisal, and goal setting are factors that improve goal attainment (Austin et al., 1996; Leivo, 2002; Renn & Fedor, 2002).
There is only a small literature on the use of evaluation and feedback in rehabilitation settings. In one controlled study (Kravetz et al., 1990) 49 males in a correctional vocational training program were randomized to receive feedback on worker trait ratings or to meet in a group to discuss the importance of worker traits. Feedback included ratings and the behaviors they were based on. Independent ratings of work performance revealed significant improvement for those receiving feedback. In a second controlled study (Hartlage & Johnsen, 1975), 75 people described as “hard-core unemployed” were randomized to receive daily video playback of work behavior or 15 minutes of daily counseling. After 15 days those receiving feedback showed greater improvement in their production, time working and their social behaviors on the job. Follow-up job placement was also better. A third controlled study (Fishwick et al., 1972) of 60 patients with schizophrenia in a rehabilitation training program compared specific feedback on speed and accuracy to non-specific feedback and found that specific feedback facilitated the acquisition of performance accuracy.
Finally, our own study involved 74 patients with schizophrenia in a transitional work program who were randomized to receive work performance feedback and goal-setting or usual services. Those receiving feedback showed greater overall improvement in work performance. Results showed that those randomized to the work feedback and goal setting condition had significantly greater improvement on the WBI with Social Skills, Cooperativeness, Personal Presentation and WBI total score being significantly greater. They also worked significantly more hours and weeks during the six-month transitional work period. Additionally, they showed greater improvements on the intrapsychic dimension of the Quality of Life scale (QLS; Heinrichs et al., 1984) that reflects increased motivation, sense of purpose, and enjoyment in life. These results indicated that specific feedback and goal setting could increase work performance, particularly for interpersonal behaviors that are less likely to be addressed by work supervisors, may increase overall productive activity, and may increase feelings of motivation, sense of purpose and enjoyment in life.
These studies vary in population, type of intervention, and work activity, but combined with the larger literature with normal workers, the research points toward the benefits of feedback and goal setting to improve work performance. In subsequent studies that employed cognitive behavioral therapy or cognitive remediation (to be described below), we have included the work feedback and goal setting groups as part of the rehabilitation services. We did so because we feel that other psychological interventions combine easily with these groups and that these feedback and goal-setting groups may be necessary to generalize the effects of these other interventions.
The Indianapolis Vocational Intervention Program: A Cognitive Behavioral Approach
The Indianapolis Vocational Intervention Program (IVIP) offers participants engaged in work activity both a weekly group and individual intervention. Together these interventions jointly target beliefs and behaviors which might interfere in their abilities to sustain work. Example of beliefs and behaviors that might lead to poor work outcomes include expectations that co-workers or supervisors will reject the participant no matter how hard they try to succeed or a tendency to be verbally aggressive when criticized. In the IVIP model, groups are generally used to teach participants didactic material. Individual sessions are used to apply those to weekly work experience.
Overall both group and individual sessions of the IVIP are based on the principles of cognitive behavior therapy (A. T. Beck, 1984). Groups are led by two co-therapists and follow a manual with a standard agenda composed of three sections: check-in, intervention and wrap-up. The primary objectives of the 10–15 minute check-in are:
to assist participants to identify potential problems at work
to give them positive social reinforcement for accomplishments
to provide a bridge from the last session
to assess how well participants understand the didactic material while reinforcing major concepts
Although the IVIP employs standard agenda items typical of cognitive behavior therapy, the group leader collaborates with participants to finalize the session agenda.
The intervention section of the group is generally 30–40 minutes and involves three activities:
teaching the week’s didactic material
assisting participants to put the didactic material into practice with some type of application exercise
giving work feedback to participants
As adapted from other sources (Burns, 1999; Linehan, 1993; Miller & Rollnick, 1991; Monti et al., 1989), the IVIP didactic curriculum is organized into four two-week modules (total of eight sessions). These are presented in order and repeated at least three times during participants’ six-month program. The content of each of these modules is summarized in Table 1. During the didactic presentation, the scheduled material is presented both abstractly and applied to participant’s actual work experiences using a wide variety of exercises. These include scripted, videotaped, and spontaneous role-play, practicing progressive muscle relaxation, and generating in-session thought records.
Table 1. Description of IVIP Group Didactic Modules | ||
|---|---|---|
Module |
Session Number and Title |
Session Objectives |
Title |
|
(examples of concepts & skills to be addressed) |
Thinking and Work |
1. Thinking Errors and |
Recognize impact of negative thinking |
|
Work |
Identify automatic thoughts that impact work |
|
2. Modifying Self-defeating Thinking |
Modify dysfunctional cognitions using 4 A model1Apply 4 A model to participants’ work experiences |
Barriers |
3. Problem Solving |
Identify existing or potential barriers to work |
To Work |
Barriers to Work 4. Coping with Emotions |
Employ steps of problem solving to work barriersDefine emotional states that threaten work Learn CBT skills to manage difficult emotions |
|
Workplace Relationships |
5. Accepting and Learning from Feedback |
Differentiate constructive and destructive criticism |
Apply steps for responding to feedback at work | ||
|
6. Effective Self-Expression |
Learn assertive communication principles |
|
|
Practice giving feedback in work settings effectively |
Realistic |
7. Thinking about |
Identify thinking errors compromising self-appraisal |
Self-Appraisal |
Capabilities & Limitations |
Identify strengths, limitations, and necessary accommodations |
|
8. Managing Success |
Define failure and success via the cognitive model Modify dysfunctional cognitions regarding work failures |
1 The 4 A model emphasizes the connections between being “aware,” “answering,” “acting” and “accepting”. | ||
Work feedback, the last aspect of the intervention section, is derived from the Work Behavior Inventory (Bryson et al., 1997), WBI feedback is given to participants every other week for the first eight weeks and then monthly. The final section of the group session is the 10 to 15-minute wrap-up during which the group leader asks participants to summarize what they have learned and/or to identify what made the most impact on them. The group leader may also provide feedback to group members about their participation in addition to bridging to the didactic topic for the next week.
The individual counseling component of the IVIP is designed to be an opportunity for participants to review and apply didactic materials from groups and to learn to identify and conceptualize concerns using the cognitive behavioral model. Sessions generally begin the week before work with the first two sessions conceived as introductory sessions. These introductory sessions have at least four objectives:
begin to establish a therapeutic alliance
orient participants to program routines and schedules
assess participants’ current expectations of work
address immediate and/or potential barriers to success at work
During this phase therapists employ primarily behavioral methods to help participants identify and overcome any initial barriers to working.
Individual sessions are comprised of the same three sections as the group session: check-in, intervention, and wrap-up. Before the therapy session begins, participants rate the strength of their conviction and extent of impact for up to four beliefs that participants and therapists have collaboratively identified. Next, during the “check-in” section, participants report the extent to which they worked on and accomplished a mutually agreed upon between-session assignment and give a brief update of the past work week including any mental health concerns. The therapist also reviews the written practice assignment from the last group session. Generally 15 minutes is needed to complete written practice assignments, with more cognitively impaired participants needing more time. As an incentive to complete the written practice assignment participants are paid for an hour of work for each completed assignment.
Rationale
As the result of several factors including the stigma of mental illness (Link et al., 1999) and the losses associated with the illness, many people with schizophrenia view themselves as having limited competence, relatively low value in the eyes of others in their community and little chance of success at work, even with help (Hays & Buckle, 1992). They may believe they have little ability to influence their lives (Hoffmann et al., 2000) and have developed a personal narrative in which failure in social and vocational contexts is expected (Lysaker & Buck, 2006).
Consistent with these observations, negative beliefs about self in schizophrenia have been found to predict poorer employment outcome (Regenold et al., 1999; Van Dongen, 1998). Indeed it seems likely that with such negative beliefs about themselves and work, many with schizophrenia enter work anticipating that difficulties will occur, see little to be gained from persevering during trying times, and therefore lose opportunities when challenges arise. The program was created to help persons with schizophrenia spectrum disorder learn to identify and monitor their own thoughts and behaviors regarding work and to give themselves an optimal chance for success. The groups assist persons to learn to understand the links between their thoughts, feelings and behaviors and the individual sessions provide them a place to explore and change how they see themselves and work.
Research Support
To date one randomized controlled study has examined the impact of the IVIP on work outcomes (Lysaker et al., 2005a). In this study, 50 participants with schizophrenia or schizoaffective disorder were recruited from a Midwestern Veterans Administration (VA) Medical Center and offered a six-month job placement and randomized to receive IVIP (n = 25) or support services (n = 25). Support services in this study were modeled after standard VA vocational support services and included a weekly group in which participants were invited to share their concerns and receive assistance with problem solving.
All participants were male and were receiving medication management by an assigned clinician. On average, participants were 48.1 years old (SD = 5.7), had 12.5 years of education (SD = 1.2), and 10.5 lifetime psychiatric hospitalizations (SD = 9.52) with the first occurring at age 24.7 (SD = 6.2). All participants were in a post-acute phase of illness as defined by having no hospitalizations or changes in psychotropic medication or housing in the month before entering the study. Participants were excluded who had a diagnosis of mental retardation or an other neurological disorder.
Following randomization, hours worked were measured weekly and job performance was assessed biweekly using the Work Behavior Inventory (WBI). Hope and self-esteem were assessed at baseline and five months using the Beck Hopelessness Scale (Beck & Steer, 1988) and Rosenberg Self Esteem Scale (Rosenberg, 1965). ANOVA revealed that participants in the IVIP group worked significantly (p < .05) more weeks than those in the support group (20.39 weeks, SD = 8.00 vs. 13.71 weeks, SD = 10.44) and had better average work performance on the WBI (WBI total 118.34, SD = 20.30 vs. WBI total 107.55, SD = 8.49). Repeated Measures ANOVA of baseline and follow-up scores indicated the IVIP group sustained initial levels of hope and self-esteem through follow-up while the support group experienced declines. Results thus provide initial evidence that the IVIP can assist persons to persist at work and to sustain their hope and enthusiasm over time. This has also been illustrated by one case report to date (Davis et al., 2005). A current randomized controlled trial is underway of 100 persons with schizophrenia spectrum disorders.
Work Place Fundamentals: A Social Skills Approach
The UCLA Social and Independent Living Skills Program is a manualized social skills training intervention for persons with SMI designed to be easily disseminated into various psychiatric rehabilitation programs (Liberman et al., 2002b; Wallace & Tauber, 2004). The overall training curriculum includes modules that teach important problem-solving skills in domains associated with independent daily living, such as medication management and interpersonal communication. Tauber and Wallace developed a self-contained module for this training program which focuses on learning and practicing fundamental problem-solving skills in the workplace as a supplement to supported employment services (Wallace & Tauber, 2004; Wallace et al., 1999).
Similar to other modules in the package, the Workplace Fundamental Skills Module includes step-by-step instructions for the clinician, a videotape demonstration of skills to be acquired, and participant handouts including workbooks with checklists and homework assignments. Instruction is provided utilizing the same behavioral teaching techniques as the other modules with the same basic “learning activities”: introduction to skill sets, videotape demonstration, role-playing with clinician and peers, step by step problem-solving to resolve lack of resources to implement skills (e.g. money, time), problem-solving to resolve disparity between learned skills and unexpected outcomes, in-vivo assignments to practice skills outside the group under the trainer’s supervision, and finally, homework assignments designed to generalize skills to the workplace. These activities are intended to explain information about problematic situations which can occur in the work environment, and then teach and repeatedly practice skills to use in the actual situation. Skills are generally taught in weekly group sessions lasting about 90 minutes with participants finishing the module in 12 to 24 sessions. There is no special training or specific educational background required to teach this program as the trainer’s manual specifies exactly what the trainer is to say and do during each session.
The overall goal of the module is to teach nine specific skills grouped into three skill sets on how to sustain employment by achieving goals that the participant and employer find equally satisfying:
Skills Set One identifies key procedures in the workplace (e.g. break times, paydays). This skill set teaches how to identify and obtain information about investments made by the participant at work, called “Gives” (time, tools, relationships, etc.), and rewards they receive when they work, called “Gets” (pay, satisfaction, etc.).
In Skill Set Two, participants are taught to “be on the alert for problems” so they can examine their work environment and develop a profile of potential problem areas, called “Sweats” (getting along with co-workers, difficult job task, etc.).
Skill Set Three is about preventing and solving problems identified in the previous set. Participants are taught how to use a general problem-solving method to prevent and solve work related problems in areas of mental and physical health, substance abuse, interactions with supervisors and co-workers, work performance, and motivation.
The core focus of the Workplace Fundamentals Module is to learn general problem-solving methods that help participants with SMI recognize and solve common workplace problems, and then implement these solutions to specific work environments. The authors note in the trainer’s manual that the module “is not focused on helping participants find a job … it does not teach skills such as obtaining job leads, producing a resume, and participating in job interviews”. The module is designed to assist people who are or will be employed and receiving supported employment or other vocational services (Wallace & Tauber, 2004).
Given the difficulties that people with schizophrenia and other persistent mental illness may have in taking what they learn in the modules and applying them to everyday life, Liberman and his colleagues developed the In Vivo Amplified Skills Training (IVAST) to enhance generalization of the modules to everyday functioning, including the workplace. IVAST uses a specialist case manager who provides tailored, community-based instruction to promote independence in the community and workplace by reducing participant reliance on case managers and therapists. A more detailed explanation of IVAST is found elsewhere (Liberman et al., 2002a).
Rationale
Although there is strong empirical evidence to show that supported employment is a worthwhile vocational approach for improving work outcome in people with persistent mental illness (Drake et al., 1996; Lehman, 1995; Mueser et al., 2004), the prevalence of social skills deficits may limit the capacity of persons to maximize the benefits from supported employment (Mueser et al., 2003; H. W. Tsang, 2002; Twamley et al., 2003b). Studies have shown that people with schizophrenia demonstrate a wide range of interpersonal deficits compared to normals, and these deficits impede the ability to function independently in the community, whether it be developing meaningful relationships, finding and keeping employment, or managing symptoms (Liberman et al., 2001; Mueser et al., 2003; Roder et al., 2001). Deficits in social skills and poor social adjustment has been recognized as a major contributor to premature job termination among persons in supported employment (D. R. Becker et al., 1998). Tenures in various work positions are comparatively short-lived for persons in supported employment (Drake et al., 1999; Mueser et al., 2004), and methods to sustain long-term employment has become increasingly important to the efficacy of the supported employment model (H. W. H. Tsang & Cheung, 2005; Wallace & Tauber, 2004).
Research Support
The empirical literature behind the UCLA Social and Independent Living Skills Program is substantial, with the programs translated into over 15 foreign languages by separate independent investigators, adapted to numerous ethnic cultures on every continent, and disseminated all over the world to hospitals, in- and out-patient programs, community centers, and day treatment programs (Chambon & Marie-Cardine, 1998; H. W. H. Tsang & Cheung, 2005). The Workplace Fundamental Module developed by Tauber and Wallace in 1999 is, however, relatively new, and investigations are only currently emerging regarding its validation and efficacy. To date, only two empirical studies have reported findings on the module in relation to supported employment and only provide weak support of its efficacy.
Wallace and Tauber (2004) conducted a randomized controlled trial to determine whether the module helped workers with severe mental illness maintain their jobs in the community compared to those receiving only supported employment. Thirty-four participants in a community mental health agency (54 % schizophrenia, 43 % bipolar) who had a history of unsuccessful job experiences ending in premature termination (fired, quit job without prospects) were randomly assigned to receive either supported employment only (n = 17) or supported employment plus the workplace skills module (n = 17). Following 18 months, preliminary analyses showed no differences in total wages earned, total hours worked, or social functioning. However, the supported employment only group had a higher rate of job turnover and was less satisfied with their jobs than those who received workplace skills training in addition to supported employment. Preliminary findings suggest that the workplace module may be a useful adjunct to supported employment services for persons with a history of unsuccessful employments.
Mueser and colleagues (2005) evaluated whether supplementary social skills training using the workplace fundamental module would improve work outcome for those recently employed through a free-standing supported employment community agency (total average days in competitive employment before entry into study was 56 ± 37). Participants were 35 persons meeting the state criteria of “severe and persistent mental illness” referred by their mental health center to the supported employment agency. Similar to the study by Wallace, participants were randomly assigned to supported employment only (n = 18) or supported employment plus the workplace fundamentals program (n = 17). Follow-up after 18 months showed no significant difference between groups on cumulative hours worked, wages earned, or days worked for first job obtained during 18 months, or all jobs obtained in 18 months. In addition, there was no difference between groups in how successfully the first job ended. The study notes that the sample population was more educated, possibly more motivated for employment, and with longer tenures on the first job compared to previous studies in supported employment, thus suggesting that the sample was in less need of social skills training. The authors suggest that “reserving workplace fundamentals program for clients who have recently experienced work-related difficulties may avoid the problem of pro-viding the intervention to clients who do not need it” (Mueser et al., 2005). Nevertheless, both studies report that employment rates were high for the workplace skills group and job turnover relatively low. The effects of supplementing supported employment services with skills training is currently under investigation with various skill programs also showing promise, including job specific skills training (Cheung & Tsang, 2005) and a cognitive social skills training milieu to enhance residential, vocational and recreational functioning (Roder et al., 2002).
Neurocognitive Enhancement Therapy: A Cognitive Remediation Approach
Neurocognitive Enhancement Therapy (NET) was developed by our group (Bell and Wexler) to directly address impairments in elemental cognitive processes that may interfere with new learning, such as occurs in vocational rehabilitation. NET is primarily comprised of computer-based training tasks with graduated levels of difficulty that require cognitive abilities often compromised in men-tal illness (e.g., attention, memory, and executive function). We have used several sources for the cognitive training exercises, and several other software packages are either available or in development. We have primarily used The Psychological Software Services CogReHab software (Bracy, 1995) which was originally developed for people with compromised brain function and modified by us for use in people with schizophrenia. The second set of exercises was developed by us in conjunction with Scientific Learning Corporation, now Positscience (www.positscience.com). Cognitive training tasks include those targeting simple attention, complex attention and response inhibition, verbal and visual memory, language mediated cognition, category formation, planning and strategy.
The approach is to have some exercises that narrowly target specific cognitive processes (re: visual reaction time), which may have associations to specific brain areas, and to have other types of exercises that use many integrated brain processes. The curriculum of exercises begins with simpler tasks and builds to more complex ones. Thus, simpler and more complex processes are exercised and integrated as training progresses. Subjects will graduate to a more difficult level when they achieve and sustain a prescribed level (e.g., 90 % correct). If performance plateaus below graduation criteria, they will be moved on to other exercises.
Cognitive training occurs in the “Cog Lab”, an attractive learning center with multiple computer work stations. Efforts are made to create an up-beat, reinforcing environment with postings of individual accomplishments and sometimes small prizes for achieving various levels of success. The cog lab is supervised by trained facilitators who provide one-to-one orientation and monitoring. Even participants who have never used a computer quickly learn the procedures. After a short time, most participants are able to work through the exercises with minimal assistance. While little is known about how much training is needed, we encourage participants to practice these exercises every day for an hour and believe that at least 40 sessions is probably the minimum necessary to achieve clinical benefit, although it takes more than 100 hours to complete the entire curriculum of exercises.
One advantage of computer-based exercises is that each participant receives the same procedure within each exercise, and the curriculum is set so that everyone proceeds systematically through the same progression of exercises. Individualization naturally results as the participant progresses quickly through a task that taps a cognitive strength and then must spend relatively more time on another that confronts a cognitive weakness.
We have incorporated these cognitive training sessions into a comprehensive rehabilitation program that includes the work performance feedback and goal setting group described previously with the addition of specific feedback about their cognitive functioning on the job. This feedback is based upon the Vocational Cognitive Rating Scale (VCRS; Greig et al., 2004) that is rated along with the WBI. Participants may set goals which relate to attention, memory or problem-solving issues that they are having on the job. The vocational specialist working with the participant may use WBI and VCRS ratings in developing supports and strategies to help the person perform better on the job. This type of follow-through is similar to the approach taken in McGurk et al.’s “Thinking Skills for Work” program (McGurk et al., 2005). Because social information processing is difficult to simulate and train on a computer, we have also incorporated a group that provides exercises for that purpose. Fuller descriptions of these interventions are available elsewhere (Bell et al., 2005; Wexler & Bell, 2005).
Rationale
Cognitive impairments are common in schizophrenia and other psychotic disorders and have been identified as “rate-limiting” factors in social and occupational domains (Liberman, 1996). Over the past few years, a number of studies have found that specific cognitive deficits predicted work performance and outcomes. McGurk and Meltzer (McGurk & Meltzer, 2000) found that better performance on executive function, working memory and vigilance distinguished full-time from part-time and unemployed work status, and found poor premorbid function, negative symptoms, and cognitive dysfunction to be significantly associated with unemployment. Bell and Bryson (2001) found that up to 79 % of the variance in improvement in work performance could be predicted from baseline cognitive performance. Evans et al. (2004) reported that baseline measures of verbal learning and memory, and symptoms of cognitive disorganization. were modestly related to work performance in a sample of 112 patients with schizophrenia enrolled in stepwise and IPS vocational rehabilitation programs. Finally, Lysaker et al. (2005b) found that participants with schizophrenia in vocational rehabilitation without impairments in processing speed and executive function showed superior work performance over time compared to participants with impairments in one or both domains. A major implication of the association between vocational disability and cognitive impairment is that remediation of cognitive deficits might improve vocational outcomes.
Evidence of brain plasticity offers a scientific foundation for cognitive remediation. The exciting possibility of restoring lost elemental brain function through cognitive retraining has gained strong support from studies of brain plasticity in non-human primates and in humans. A review of advances in brain plasticity research by Mark Hallett (2004), Chief of Medical Neurology Branch National Institute of Neurological Disease at NIH, indicates compelling evidence for the brain as a self-organizing, experience-based organ that responds rapidly at cellular and molecular levels to environmental change. Hallet abstracts several basic principles from the literature. The first is that there is competition between body parts for representation in the central nervous system, and changes can occur rapidly. A second principle is that use of a body part increases representation and disuse decreases representation as seen for example in a study of a group of people with broken ankles after a ski accident who lost representation of the body part because of its immobility. A third basic principle is that there is multimodal plasticity. For example, Braille readers whose blindness occurred before age 13 activated the visual cortex when reading, and with TMS inhibition of the occipital lobe, they could no longer read Braille. Recovery in stroke patients is due to brain plasticity. In a study of stroke patients with hemiparesis who had a full recovery, neuroimaging revealed that this had occurred through a reorganization of the cortex.
There are several examples of clinical applications of these principles outside of psychiatry. Constraint-induced movement therapy (CIMT; Taub & Morris, 2001) has been shown to produce better post-stroke hemiparesis rehabilitation by restraining the unaffected limb and performing six hours/day of intensive task practice aimed at the impaired upper extremity. In a review paper (Taub et al., 2003) the authors attribute the improvement to two separate but linked mechanisms, overcoming learned non-use and facilitating use-dependent cortical reorganization. Auditory discrimination training for people receiving hearing aids boosted their ability to process sound from noise because hearing loss had decreased cortical representation of those sounds and hearing aides alone, while providing a clearer input, did not increase perception. Eight weeks of computer-based training significantly increased auditory discrimination over amplification alone (Stecker et al., 2006). Perceptual learning through computer-based training can drive neuronal reorganization in visual and auditory modalities, and it has been effectively applied to central auditory processing disorder and dyslexia (Cohen et al., 2005; Merzenich et al., 1996).
As these examples illustrate, neuroplasticity research is spawning new approaches to rehabilitation. In schizophrenia and other mental illnesses, the basic mechanisms of overcoming learned non-use and facilitating use-dependent cortical reorganization may have application. Regarding learned non-use, it is very likely that “disuse atrophy” of associated neural resources occurs because patients avoid situations that tax cognitive weaknesses so these cognitive functions go unexercised and unrewarded. By using simple computer-based cognitive exercises and building up to more complicated problem-solving, cognitive remediation forces patients to employ cognitive processes that they would otherwise avoid, thus reversing learned non-use. This vigorous exercising of cognitive functions may thus facilitate use-dependent cortical reorganization.
Research Support
Several literature reviews of cognitive remediation have been published (Bellack et al., 1999; Kurtz et al., 2001; Pilling et al., 2002; Rund & Borg, 1999; Suslow et al., 2001; Twamley et al., 2003a). All but the Pilling review concluded that the literature favored clinical benefit of one type or another. Twamley provided the most comprehensive review of randomized clinical trials and found 17 randomized clinical trials in the literature, and calculated weighted mean effect sizes (Cohen’s d) for improvements in neuropsychological performance = .32, for reductions in symptom severity = .26 and for improvements in everyday function = .51 (Twamley et al., 2003a).
We have conducted two randomized clinical trials that combine our NET training with work services. The first was performed at the VA Connecticut Healthcare System and involved six months of NET plus work therapy (NET+WT) compared with WT alone (n =145). The second was at the Connecticut Mental Health Center and involved a year of active intervention that included NET plus supported employment (NET+SE) compared with SE alone (n = 76). Participants in both studies were diagnosed with schizophrenia or schizoaffective disorder and were in outpatient treatment. Details of method are available elsewhere (Bell et al., 2001; Wexler & Bell, 2005).
In these studies we reasoned that if NET is effective, there should be a chain of effects from the most proximal to the cognitive training, (i.e. improvement on the trained tasks), to more distal ones including work outcomes. In a series of published reports we found that participants receiving NET improved on training tasks and that almost half of those with significant clinical deficits on working memory tasks reached normal levels of performance by the conclusion of training (Bell et al., 2003). We tested the generalization of the training to similar but untrained tasks on neuropsychological testing and found significantly greater improvement for those receiving NET at the conclusion of training (Bell et al., 2001). We subsequently found that these improvements endured for six-months after the end of the active training (Fiszdon et al., 2004). We also have unpublished evidence that those receiving NET showed greater improvement in work performance (WBI scores) and cognitive performance on the job (VCRS scores) during the active interventions. Most importantly, work outcomes were better for those receiving NET with their work services. In the VA study, those in NET+WT worked significantly more hours (p < .05) and earned more money during the six months following the intervention (Figure 1).
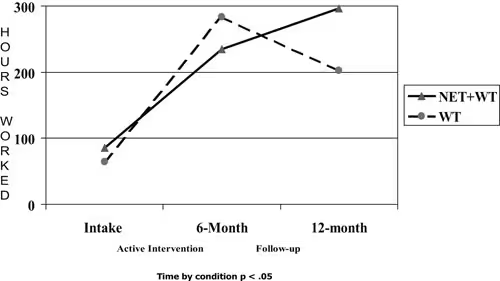
Figure 1. Hours worked by condition for the 6 months prior to intake, 6 months of active intervention and 6 months follow-up
In the CMHC study, we found that NET combined with supported employment led to significantly more hours (p < .05) worked during the 12 months after the intervention (transitional and competitive employment combined hours) and significantly higher rates (p < .05) of obtaining competitive employment (Wexler & Bell, 2005) (see Figure 2 and Figure 3).

Figure 1. Hours worked by condition over two years

Figure 3. Cumulative rates of competitive employment
Taken together these findings suggest that cognitive retraining can have significant functional benefits when included in a comprehensive rehabilitation program that affords opportunity to acquire practical new learning. We believe that cognitive training improves cognitive processing and thereby makes it possible for participants to gain more from other forms of rehabilitation.
Over the past several years we have been gratified to see our work be adopted and extended by our colleagues. McGurk, Mueser and Pascaris (McGurk et al., 2005) have recently published the first small (n = 44) effectiveness study combining supported employment with cognitive training. Their intervention was based at two vocational agencies servicing mental health clients. They used supported employment augmented with CogPak training (www.cogpack.com) and a follow-through method of having the cognitive training specialist consult regularly with the employment specialist to discuss “job supports to address cognitive challenges on the job”. This is a useful variation of our approach of providing feedback to the patient and job specialist about cognitive performance on the job and setting goals to address such problems. They call their program “Thinking Skills for Work”. Clients with severe mental illness who had had a previous job failure were randomized to receive supported employment or supported employment augmented with their program. Cognitive and psychopathology assessments were conducted at three months (the conclusion of their cognitive intervention) and employment data were collected for one year. Results were remarkable. Those receiving the cognitive augmentation showed significantly greater improvement on cognitive functioning and on depression and autistic preoccupation scores on the PANSS. Clients receiving cognitive augmentation worked more hours and earned more wages. Most importantly, 69.6 % achieved competitive employment as compared with only 4.8 % of those receiving supported employment alone (p = .000). They attributed the very low rate for their control condition to their selection criteria, which consisted of patients with prior vocational failures.
Discussion
Those looking for ways to improve the lives of people recovering from persistent and severe mental illness may find excitement and hope in the programs that have been presented in this report. Supported employment and other work services offer opportunities for community reintegration through the constructive social roles that working provides. For some, working may lead to reduced symptoms, greater self-esteem and a higher quality of life.
The four interventions that we have described address overlapping but distinct areas of impairment that accompany mental illness and that may be barriers to achieving work success. Work feedback with goal setting compensates for impairments in self monitoring and social perception and enhances motivation and problem solving. The IVIP focuses on negative cognitions and improves coping. Work Place Fundamentals attempts to teach social skills in common areas of weakness that may be particularly challenged in work life. And, cognitive remediation attempts to restore elemental cognitive functions that have been impaired by illness so that new learning through rehabilitation may occur. Each of these approaches has a sound rationale and at least some evidence of efficacy. Most have a manual or a systematic description that make it possible to replicate the methods in other settings.
There is every reason to believe that a comprehensive approach to vocational rehabilitation could combine these interventions to the benefit of the patient. We are not yet at the point where we can be prescriptive about exactly what methods to apply to which patients, and some of these interventions may be better suited to some settings than to others. Yet, there is sufficient evidence to warrant clinicians and vocational specialists, using their own judgment, to enhance their existing work services with these psychological approaches. It is the hope that these interventions will allow people with mental illness to more speedily and effectively reintegrate into their community so that they may lead more satisfying lives.
MORRIS BELL |
|---|
Morris Bell, Ph.D., is a Research Career Scientist for the Department of Veterans Affairs, Rehabilitation Research & Development Service and Professor of Psychiatry at Yale University School of Medicine. “Exploring Ways to Restore Cognitive and Work Capacity” is the mission statement of his research program. The goal is to restore functional capacity to patients with a wide range of psy-chiatric conditions. Research has been particularly focused on vocational rehabilitation and neurocognitive rehabilitation and has included testing interventions that can augment current best practices. |
|
Key publications Bell, M. D., & Bryson, G. (2001). Work rehabili-tation in schizophrenia: does cognitive impair-ment limit improvement? Schizophrenia Bulletin, 27, 269–279. Bell, M., Bryson, G., Greig, T., Corcoran, C., & Wexler, B. E. (2001). Neurocognitive enhancement therapy with work therapy: effects on neuropsychological test performance. Archives of General Psychiatry, 58, 763–768. Bell, M. D., Bryson, G. J., Greig, T. C., Fiszdon, J. M., & Wexler, B. E. (2005). Neurocognitive enhancement therapy with work therapy: productivity outcomes at 6- and 12-month follow-ups. Journal of Rehabilitation Research and Development, 42, 829–838. |
JIMMY CHOI |
|---|
Jimmy Choi, Ph.D., is a Research Neuropsychologist at the VA Connecticut Healthcare System and Associate Research Scientist at the Yale University School of Medicine. He is currently conducting research into the neurophysiology of schizophrenia using pupillometry, motivational models of learning in neuropsychiatry, use of atypical neuroleptics to enhance cognitive remediation, development of computerized cognitive training software, and rehabilitation of early Alzheimer’s disease. |
|
Key publications Choi, J., & Medalia, A. (2005). Factors associated with a positive response to cognitive remediation in a community psychiatric sample. Psychiatric Services, 56, 602–604. Fiszdon, J. M., Choi, J., Bryson, G. J., & Bell, M. D. (2006). Impact of intellectual status on response to cognitive task training in patients with schizophrenia. Schizophrenia Research, 87, 261–269. |
PAUL LYSAKER |
|---|
Paul Lysaker, Ph.D., is a staff psychologist at the Roudebush VA Medical Center and Associate Clinical Professor of Clinical Psychology at Indiana University School of Medicine Department of Psychiatry. He is widely published in the areas of psychotherapy and recovery for persons with schizophrenia. |
|
Key publications Davis, L. W., Lysaker, P. H., Lancaster, R. S., Bryson, G. J., & Bell, M. D. (2005). The Indianapolis Vocational Intervention Program: a cognitive behavioral approach to addressing rehabilitation issues in schizophrenia. Journal of Rehabilitation Research & Development, 42, 35–45. Lysaker, P. H., Bond, G., Davis, L. W., Bryson, G. J., & Bell, M. D. (2005). Enhanced cognitive behavioral therapy for vocational rehabilitation in schizophrenia: Effects on hope and work. Journal of Rehabilitation Research and Development, 42, 673–682. Lysaker, P. H., & Buck, K. D. (2006). Narrative enrichment in the psychotherapy for persons with schizophrenia: a single case study. Issues in Mental Health Nursing, 27, 233–247. |
Referanser
References
Austin, J., Kessler, M. L., Riccobono, J. E., & Bailey, J. S. (1996). Using feedback and reinforcement to improve the performance and safety of a roofing crew. Journal of Organizational Behavior Management, 16, 49–75.
Balcazar, F. R., Hopkins, B. L., & Suarez, Y. (1986). A critical, objective review of performance feedback. Journal of Organizational BehaviorManagement, 7, 65–89.
Beck, A. T. (1984). Cognition and therapy. Archives of General Psychiatry, 41, 1112–1115.
Beck, A. T., & Steer, R. A. (1988). The beck hopelessness scale manual. Psychological Corp., San Antonio, TX.
Becker, D. (2002). Supported employment toolkit. Lebanon, NH: Psychiatric Research Center.
Becker, D. R., Drake, R. E., Bond, G. R., Xie, H., Dain, B. J., & Harrison, K. (1998). Job terminations among persons with severe mental illness participating in supported employment. Community Mental Health Journal, 34 (1), 71–82.
Bell, M., Bryson, G., Greig, T., Corcoran, C., & Wexler, B. E. (2001). Neurocognitive enhancement therapy with work therapy: Effects on neuropsychological test performance. Archives of General Psychiatry, 58, 763–768.
Bell, M., Bryson, G., & Wexler, B. E. (2003). Cognitive remediation of working memory deficits: Durability of training effects in severely impaired and less severely impaired schizophrenia. Acta Psychiatrica Scandinavica, 108 (2),101–109.
Bell, M. D., & Bryson, G. (2001). Work rehabilitation in schizophrenia: Does cognitive impairment limit improvement? Schizophrenia Bulletin, 27, 269–279.
Bell, M. D., Bryson, G. J., Greig, T. C., Fiszdon, J. M., & Wexler, B. E. (2005). Neurocognitive enhancement therapy with work therapy: Productivity outcomes at 6- and 12-month follow-ups. Journal of Rehabilitation Research and Development, 42, 829–838.
Bellack, A. S., Gold, J. M., & Buchanan, R. W. (1999). Cognitive rehabilitation for schizophrenia: Problems, prospects, and strategies. Schizophrenia Bulletin, 25, 257–274.
Bolton, B., & Roessler, R. (1986). Manual for the work personality profile. Fayetville, AK: Arkansas Research and Training Center in Vocational Rehabilitation.
Bond, G. R., Becker, D. R., Drake, R. E., Rapp, C. A., Meisler, N., Lehman, A. F., et al. (2002). Implementing supported employment as an evidence-based practice. Psychiatric Services, 52, 313–322.
Bracy, O. (1995). Cogrehab software. Indianapolis, Indiana: Psychological Software Services.
Bryson, G., Bell, M. D., Greig, T., & Kaplan, E. (1999). The work behavior inventory: Prediction of future work success of people with schizophrenia. Psychiatric Rehabilitation Journal, 23 (2), 113–117.
Bryson, G., Bell, M. D., Lysaker, P., & Zito, W. (1997). The work behavior inventory: A scale for the assessment of work behavior for people with severe mental illness. Psychiatric Rehabilitation Journal, 20 (4), 47–55.
Burns, D. D. (1999). The feeling good handbook (Revised Edition.). New York: Penguin Group.
Chambon, O., & Marie-Cardine, M. (1998). An evaluation of social skills training modules with schizophrenia inpatients in france. International Review of Psychiatry, 10 (1), 26–29.
Cheung, L. C., & Tsang, H. W. (2005). Factor structure of essential social skills to be salespersons in retail market: Implications for psychiatric rehabilitation. Journal of Behavior Therapy and Experimental Psychiatry, 36, 265–280.
Clark, R. E., Xie, H., Becker, D. R., & Drake, R. E. (1998). Benefits and costs of supported employment from three perspectives. Journal of Behavioral Health Services & Research, 25(1), 22–34.
Cohen, W., Hodson, A., O'Hare, A., Boyle, J., Durrani, T., McCartney, E., et al. (2005). Effects of computer-based intervention through acoustically modified speech (fast forword) in severe mixed receptive-expressive language impairment: Outcomes from a randomized controlled trial. Journal of Speech Language & Hearing Research, 48, 715–729.
Cook, J. A., Leff, H. S., Blyler, C. R., Gold, P. B., Goldberg, R. W., Mueser, K. T., et al. (2005). Results of a multisite randomized trial of supported employment interventions for individuals with severe mental illness. Archives of General Psychiatry, 62, 505–512.
Davis, L. W., Lysaker, P. H., Lancaster, R. S., Bryson, G. J., & Bell, M. D. (2005). The indianapolis vocational intervention program: A cognitive behavioral approach to addressing rehabilitation issues in schizophrenia. Journal of Rehabilitation Research & Development, 42 (1), 35–45.
Drake, R. E., McHugo, G. J., Bebout, R. R., Becker, D. R., Harris, M., Bond, G. R., et al. (1999). A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Archives of General Psychiatry, 56, 627–633.
Drake, R. E., McHugo, G. J., Becker, D. R., Anthony, W. A., & Clark, R. E. (1996). The new hampshire study of supported employment for people with severe mental illness. Journal of Consulting & Clinical Psychology, 64, 391–399.
Evans, J. D., Bond, G. R., Meyer, P. S., Kim, H. W., Lysaker, P. H., Gibson, P. J., et al. (2004). Cognitive and clinical predictors of success in vocational rehabilitation in schizophrenia. Schizophrenia Research, 70, 331–342.
Fishwick, L. V., Ayer, M. J., & Butler, A. J. (1972). The effects of specific and general feedback information on the speed and accuracy of schizophrenic work performance. Journal of Clinical Psychology, 28, 581–583.
Fiszdon, J. M., Bryson, G. J., Wexler, B. E., & Bell, M. D. (2004). Durability of cognitive remediation training in schizophrenia: Performance on two memory tasks at 6-month and 12-month follow-up. Psychiatry Research, 125 (1), 1–7.
Greig, T., Bryson, G. J., & Bell, M. D. (2004). Development of a scale for the assessment of cognitive impairments in vocational rehabilitation: Reliability and predictive validity. Journal of Vocational Rehabilitation, 21, 71–81.
Hallett, M. (2004, May 1). The plastic brain. Paper presented at the Society of Biological Psychiatry, New York.
Hartlage, L., & Johnsen, R. (1975). Video playback as a rehabilitation tool with the hard-core unemployed. Rehabilitation Psychology, 20, 116–120.
Hays, J. R., & Buckle, K. E. (1992). Self-efficacy among hospitalized mentally ill patients. Psychological Reports, 70 (1), 57–58.
Heinrichs, D. W., Hanlon, T. E., & Carpenter, W. T., Jr. (1984). The quality of life scale: An instrument for rating the schizophrenic deficit syndrome. Schizophrenia Bulletin, 10, 388–398.
Hoffmann, H., Kupper, Z., & Kunz, B. (2000). Hopelessness and its impact on rehabilitation outcome in schizophrenia – an exploratory study. Schizophrenia Research, 43, 147–158.
Kravetz, S., Florian, V., & Nofer, E. (1990). The differential effects of feedback of trait ratings on worker traits in vocational rehabilitation workshops in a correctional institution. Vocational Evaluation & Work Adjustment Bulletin, 23(2), 47–54.
Kurtz, M. M., Moberg, P. J., Gur, R. C., & Gur, R. E. (2001). Approaches to cognitive remediation of neuropsychological deficits in schizophrenia: A review and meta-analysis. Neuropsychology Review, 11 (4), 197–210.
Lehman, A. F. (1995). Vocational rehabilitation in schizophrenia. Schizophrenia Bulletin, 21, 645–656.
Lehman, A. F., & Steinwachs, D. M. (1998). Patterns of usual care for schizophrenia: Initial results from the schizophrenia patient outcomes research team (port) client survey. Schizophrenia Bulletin, 24 (1), 11–20; discussion 20–32.
Leivo, A. K. (2002). A field study of the effects of gradually terminated public feedback on housekeeping performance. Journal of Applied Social Psychology, 31, 1184–1203.
Liberman, R. (1996). "Rate-limiting" factors in work capacity in schizophrenia: Psychopathology and neurocognitive deficits. Paper presented at the Vocational Rehabilitation Research Colloquium, Boston, MA.
Liberman, R. P., Eckman, T. A., & Marder, S. R. (2001). Rehab rounds: Training in social problem solving among persons with schizophrenia. Psychiatric Services, 52, 31–33.
Liberman, R. P., Glynn, S., Blair, K. E., Ross, D., & Marder, S. R. (2002a). In vivo amplified skills training: Promoting generalization of independent living skills for clients with schizophrenia. Psychiatry, 65, 137–155.
Liberman, R. P., Wallace, C. J., & Robertson, M. J. (2002b). Dissemination of skills training. Psychiatric Services, 53, 215.
Linehan, M. M. (1993). Dialectical behavior therapy for treatment of borderline personality disorder: Implications for the treatment of substance abuse. NIDA Research Monograph, 137, 201–216.
Link, B. G., Phelan, J. C., Bresnahan, M., Stueve, A., & Pescosolido, B. A. (1999). Public conceptions of mental illness: Labels, causes, dangerousness, and social distance. American Journal of Public Health, 89, 1328–1333.
Locke, E. A., & Latham, G. P. (2002). Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. American Psychologist, 57, 705–717.
Lysaker, P. H., Bond, G., Davis, L. W., Bryson, G. J., & Bell, M. D. (2005a). Enhanced cognitive behavioral therapy for vocational rehabilitation in schizophrenia: Effects on hope and work. Journal of Rehabilitation Research and Development, 42, 673–682.
Lysaker, P. H., Bryson, G. J., Davis, L. W., & Bell, M. D. (2005b). Relationship of impaired processing speed and flexibility of abstract thought to improvements in work performance over time in schizophrenia. Schizophrenia Research, 75, 211–218.
Lysaker, P. H., & Buck, K. D. (2006). Narrative enrichment in the psychotherapy for persons with schizophrenia: A single case study. Issues in Mental Health Nursing, 27, 233–247.
McGurk, S. R., & Meltzer, H. Y. (2000). The role of cognition in vocational functioning in schizophrenia. Schizophrenia Research, 45, 175–184.
McGurk, S. R., Mueser, K. T., & Pascaris, A. (2005). Cognitive training and supported employment for persons with severe mental illness: One-year results from a randomized controlled trial. Schizophrenia Bulletin, 31, 898–909.
Merzenich, M. M., Jenkins, W. M., Johnston, P., Schreiner, C., Miller, S. L., & Tallal, P. (1996). Temporal processing deficits of language-learning impaired children ameliorated by training. Science, 271, 77–81.
Miller, W. R., & Rollnick, S. (1991). Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press.
Monti, P. M., Abrams, D. B., Kadden, R. M., & Cooney, N. L. (1989). Treating alcohol dependence: A coping skills training guide. New York: Guilford Press.
Mueser, K. T., Aalto, S., Becker, D. R., Ogden, J. S., Wolfe, R. S., Schiavo, D., et al. (2005). The effectiveness of skills training for improving outcomes in supported employment. Psychiatric Services, 56, 1254–1260.
Mueser, K. T., Clark, R. E., Haines, M., Drake, R. E., McHugo, G. J., Bond, G. R., et al. (2004). The hartford study of supported employment for persons with severe mental illness. Journal of Consulting & Clinical Psychology, 72, 479–490.
Mueser, K. T., Salyers, M. P., & Mueser, P. R. (2001). A prospective analysis of work in schizophrenia. Schizophrenia Bulletin, 27, 281–296.
Mueser, K. T., Torrey, W. C., Lynde, D., Singer, P., & Drake, R. E. (2003). Implementing evidence-based practices for people with severe mental illness. Behavior Modification, 27, 387–411.
Pilling, S., Bebbington, P., Kuipers, E., Garety, P., Geddes, J., Orbach, G., et al. (2002). Psychological treatments in schizophrenia: I. Meta-analysis of family intervention and cognitive behaviour therapy. Psychological Medicine, 32, 763–782.
Prue, D. M., & Fairbank, J. A. (2002). Performance feedback in organizational behavior management: A review. Journal of Organizational Behavior Management, 3(1), 1–16.
Razzano, L. A., Cook, J. A., Burke-Miller, J. K., Mueser, K. T., Pickett-Schenk, S. A., Grey, D. D., et al. (2005). Clinical factors associated with employment among people with severe mental illness: Findings from the employment intervention demonstration program. Journal of Nervous & Mental Disease, 193, 705–713.
Regenold, M., Sherman, M. F., & Fenzel, M. (1999). Getting back to work: Self-efficacy as a predictor of employment outcome. Psychiatric Rehabilitation Journal, 22, 361–367.
Renn, R. W., & Fedor, D. B. (2002). Development and field test of a feedback seeking, self-efficacy, and goal setting model of work performance. Journal of Management, 27, 563–583.
Roder, V., Brenner, H. D., Muller, D., Lachler, M., Zorn, P., Reisch, T., et al. (2002). Development of specific social skills training programmes for schizophrenia patients: Results of a multicentre study. Acta Psychiatrica Scandinavica, 105, 363–371.
Roder, V., Zorn, P., Muller, D., & Brenner, H. D. (2001). Improving recreational, residential, and vocational outcomes for patients with schizophrenia. Psychiatric Services, 52, 1439–1441.
Rosenberg, M. (1965). Society and the adolescent child. Princeton, NJ: Princeton University Press.
Rund, B. R., & Borg, N. E. (1999). Cognitive deficits and cognitive training in schizophrenic patients: A review. Acta Psychiatrica Scandinavica, 100, 85–95.
Stecker, G. C., Bowman, G. A., Yund, E. W., Herron, M. A., Roup, C. M., & Woods, D. L. (2006). Perceptual training improves syllable identification in new and experienced hearing aid users. Journal of Rehabilitation Research & Development, 43, 537–552.
Suslow, T., Schonauer, K., & Arolt, V. (2001). Attention training in the cognitive rehabilitation of schizophrenic patients: A review of efficacy studies. Acta Psychiatrica Scandinavica, 103, 15–23.
Taub, E., & Morris, D. M. (2001). Constraint-induced movement therapy to enhance recovery after stroke. Current Atherosclerosis Reports, 3, 279–286.
Taub, E., Uswatte, G., & Morris, D. M. (2003). Improved motor recovery after stroke and massive cortical reorganization following constraint-induced movement therapy. Physical Medicine & Rehabilitation Clinics of North America, 14 (1 Suppl), S77–S91.
Tsang, H. W. (2002). Problem solving skills and social skills training. Psychiatric Services, 53, 1034.
Tsang, H. W. H., & Cheung, L. C. C. (2005). Social skills training for people with schizophrenia: Theory, practice and evidence. In J. E. Pletson (Ed.), Progress in Schizophrenia Research (ss. 181–207). Hauppauge, NY: Nova Science Publishers.
Twamley, E. W., Jeste, D. V., & Bellack, A. S. (2003a). A review of cognitive training in schizophrenia. Schizophrenia Bulletin, 29, 359–382.
Twamley, E. W., Jeste, D. V., & Lehman, A. F. (2003b). Vocational rehabilitation in schizophrenia and other psychotic disorders: A literature review and meta-analysis of randomized controlled trials. Journal of Nervous & Mental Disease, 191, 515–523.
Van Dongen, C. J. (1998). Self-esteem among persons with severe mental illness. Issues in Mental Health Nursing, 19, 29–40.
Wallace, C. J., & Tauber, R. (2004). Supplementing supported employment with workplace skills training. Psychiatric Services, 55, 513–515.
Wallace, C. J., Tauber, R., & Wilde, J. (1999). Teaching fundamental workplace skills to persons with serious mental illness. Psychiatric Services, 50, 1147–1149.
Wexler, B. E., & Bell, M. D. (2005). Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophrenia Bulletin, 31, 931–-941.
